State Rep. Wendi Thomas will never forget a jarring phone call she received from a distraught mother, whose 16-year-old daughter had thoughts of self-harm. According to Thomas, despite this mom spending multiple days calling over 40 offices, the first available appointment with a mental health provider wasn’t for 30 days.
This year in Pennsylvania, 1.8 million individuals are reporting that they have a mental illness, from anxiety and depression to bipolar disorder and addiction. However, 1.7 million of that population live in an area that doesn’t have enough mental health professionals.
“When these mental health conditions are not treated, we end up with people in our emergency rooms,” said Thomas, who said ERs are only able to deliver high-cost, crisis management care.
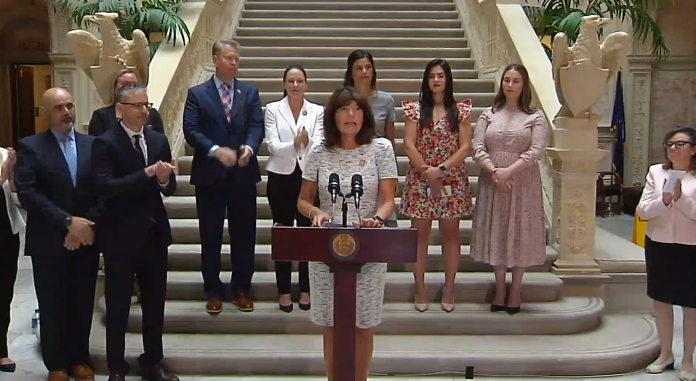
Last Wednesday, Thomas hosted a press conference to announce legislation that would improve access through a Collaborative Care Model, which would deliver timely psychiatric care in the primary care setting.
“House Bill 2686 will set up the ability for the primary care doctor to get a state-funded grant to integrate behavioral health into their practice. The grant program will be used to cover the start-up cost for small and solo primary care physicians,” said Thomas.
Though a Collaborative Care Model is already successfully implemented at larger healthcare systems, such as Penn Medicine, and Medicaid, Medicare and most insurance providers cover it, small primary care physicians lack the time and support to get the model up and running. House Bill 2686 would allocate money from the American Rescue Plan to ensure approximately 100 providers are able to launch it.
Present at the press conference was Hope Selarnick, MD, president of the Pennsylvania Psychiatric Society, who explained how exactly the Collaborative Care Model operates.
A “care team” is led by a primary care provider and includes a consulting psychiatrist and behavioral healthcare manager. The team cares for a defined group of patients and closely tracks each patient’s progress using an evidence- and measurement-based care plan.
Selarnick shared that 80 patients can be part of the Collaborative Care Model at any given time, a drastic uptick from the handful of patients a psychiatrist typically sees in their office on a daily basis. Not only does the model increase access to mental health services, said Selarnick, it also decreases hospitalization rates.
“When people feel well mentally, they take better care of themselves physically,” she stated.

In 2021, the nation saw more than 100,000 overdose-related deaths – the highest ever reported. In Pennsylvania alone that year, there were over 5,000 overdose deaths and 2,000 suicides, the second leading cause of death for ages 10-34. Selarnick stressed that the COVID-19 pandemic has exacerbated an ever-growing mental health crisis among youth, and that the Collaborative Care Model would get them the help they need in a timely manner…not in 30 days like the daughter of Thomas’ constituent.
“Most mental health issues, such as mild to moderate depression, anxiety and alcohol use disorder can be treated within a primary care setting,” said Selarnick. “How do we expand on this? The solution is the Collaborative Care Model, which expands access to care exponentially. CoCM is patient-centered and evidence-based. The Pennsylvania Psychiatric Society embraces CoCM as the most viable solution to date. It is vital to support H.B. 2686 for the health of our citizens in the commonwealth.”
Matthew Press, MD, MSc, physician executive, Penn Primary Care, reflected on when Penn Medicine implemented the model. Though they expected about 500 patients to seek help, they ended up serving over 30,000.
“For too long, primary care physicians have struggled to provide high-quality, accessible, affordable and coordinated mental health care to our patients,” said Press. “Collaborative Care is a proven solution, and our experience implementing it at Penn Medicine has been transformational.”
Ultimately, Thomas’ goal with H.B. 2686 is to move the healthcare system forward to a holistic approach, where mental health issues can be treated at a time when the person can heal – not in an emergency room when they’re already in crisis. She said this approach would also allow individuals to feel more comfortable and less stigmatized in seeking help.
State Rep. Frank Farry, chair of the Human Services Committee, where the bill has been assigned, was in attendance at the press conference. He praised his fellow Bucks County legislator for tackling mental health throughout her tenure in office.
“I commend Rep. Thomas’ work on this bill to make a Collaborative Care Model of treatment more accessible to those in crisis,” said Farry. “As chairman of the House Human Services Committee, I look forward to advocating for programs such as this to help those in need of better, more directed care.”
Samantha Bambino can be reached at [email protected]